National Issues
Part 4 of 4: Post EBOLA – Exploring a National Disease Surveillance System for Nigeria
Learning from eHealth experiences in other countries over the past 30 years: in order that Nigeria may avoid the costly mistakes of others
BACKGROUND:
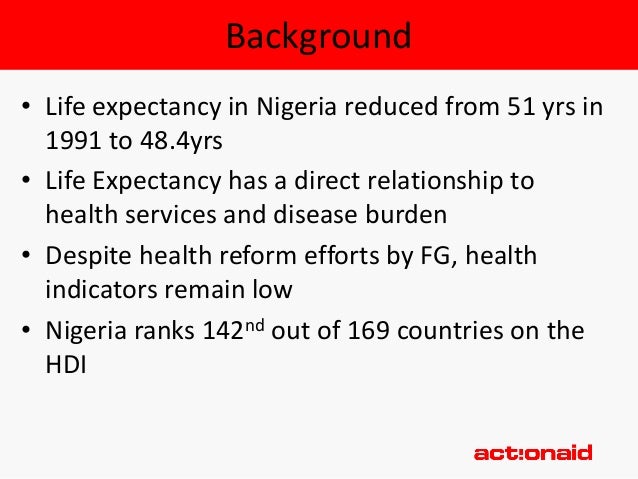
In my three previous articles, Post EBOLA – Exploring a National Disease Surveillance System for Nigeria Part 1, Part 2 and Part 3, I introduced the real need for Nigeria to have a national Health eSurveillance System for for diseases like Ebola, HIV, Tuberculosis, Malaria amongst others. Additionally, I explored the massive economic benefits that will accrue to Nigeria by having a healthier population resulting from an enhanced health system based on accurate and timely information derived from eHealth systems. This economic benefit was calculated based on the 2001 UN WHO report ‘Macroeconomics and Health: Investing in Health for Economic Development’.
In the third article I addressed the big challenge in this journey – given all of the components of a national health system, where is the best place to start? This is particularly challenging in the subject area of Health Informatics which all too often is seen to be a task that is straightforward, which in fact is not at all the case. In order to put this reality in perspective a visit to the site ‘Grand Engineering Challenges of the 21st Century’ is recommended. Published by the National Academy of Engineering in the USA the site lists among the 14 Grand Challenges: ‘Reverse-engineer the brain’, and the one that we are exploring ‘Improve Health Informatics’.
Insofar as there is ample evidence of what many other countries have achieved in eHealth, and where many expensive eHealth failures have been documented, it is prudent to take a closer look at this history that spans over 30 years, to ‘learn from history’ in order to lessen the chance of failure, and of course to raise the chance of success. What are the key factors for success, which when addressed, can assist in avoiding failure in Health Informatics?
Some on-line literature/references on failures to achieve SUCCESS in eHealth
Let’s start with the reality of this complex field of activity – Health Informatics.
- ‘There are many more failure stories to tell than there are success stories’
M. Berg, Implementing information systems in health care organizations: myths and challenges, Int. J. Med. Inform. 64 (2001) 143—156.
- “The generalised assumption of health information systems (HIS) success is questioned by a few commentators in the medical informatics field. They point to widespread HIS failure. The purpose of this paper was therefore to develop a better conceptual foundation for, and practical guidance on, health information systems failure (and success).”
Richard Heeks, U of Manchester International Journal of Medical Informatics (2006) 75, 125
http://www.uio.no/studier/emner/matnat/ifi/INF5761/v12/undervisningsmateriale/Heeks%20-%202006%20-20Health%20information%20systems%20Failure,%20success%20and%20i.pdf
- “For example, in the Philippines, an aid-funded project to introduce a public health services information system was designed according to a Western model that assumed the presence of skilled programmers, skilled project managers, a sound technological infrastructure, and a need for information outputs like those used in an American health care organisation. In reality, none of these was present in the Philippine context and the information system failed.“
R. Jayasuriya, Managing information systems for health services in a developing country, Int. J. Inform. Manage. 19 (1999) 335—349.
- This report is on the failure of a large (about US$50 million) HIS initiative in Limpopo Province, South Africa in 1998 – 2002.
“Why are computerised health information systems prone to failure?
• Failure to take into account the social and professional cultures of healthcare organisations and to recognise that education of users and computer staff is an essential precursor
• Underestimation of the complexity of routine clinical and managerial processes
• Dissonance between the expectations of the commissioner, the producer, and the users of the system
• Implementation of systems is often a long process in a sector where managerial change and corporate memory is short
• “My baby” syndrome
• Reluctance to stop putting good money after bad
• Failure of developers to look for and learn lessons from past projects
You can get a copy of the repot here: BMJ VOLUME 326 19 APRIL 2003 bmj.com 861
FACTORS leading to SUCCESS for eHealth in DEVELOPING COUNTRIES
As we see in the few references included to eHealth failures above in the developing countries – and even many more in the developed countries – including a US$20 billion failure at the UK NHS between 2002 and 2012, there are many pitfalls to avoid in the implementation of eHealth in Nigeria, starting with the Heron PAS/eSurveillance (Ebola, and other health conditions).
# 1 ECONOMICS/HEALTH BUDGET
This is by far the most critical matter to take into account, and to manage carefully on an on-going basis. Unfortunately, this key factor is often overlooked, leading to failure when the actual costs for such future matters as on-going support for hardware, software, and technical matters escalate beyond what the country annual public health budget can cope with.
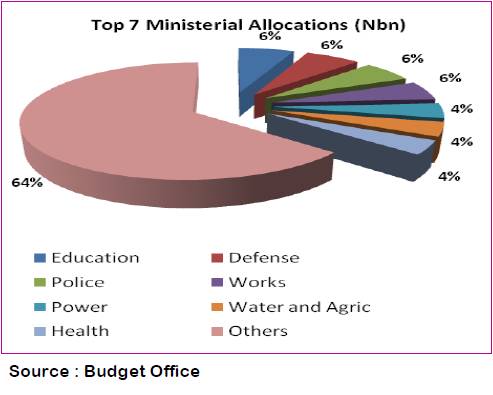
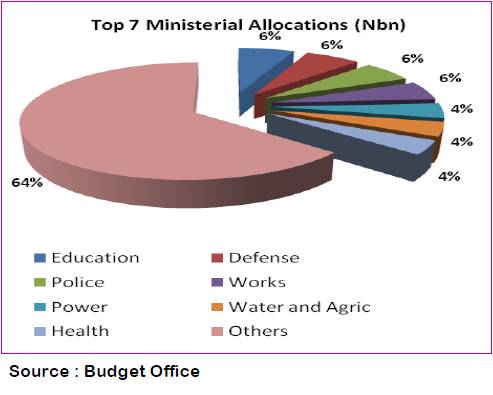
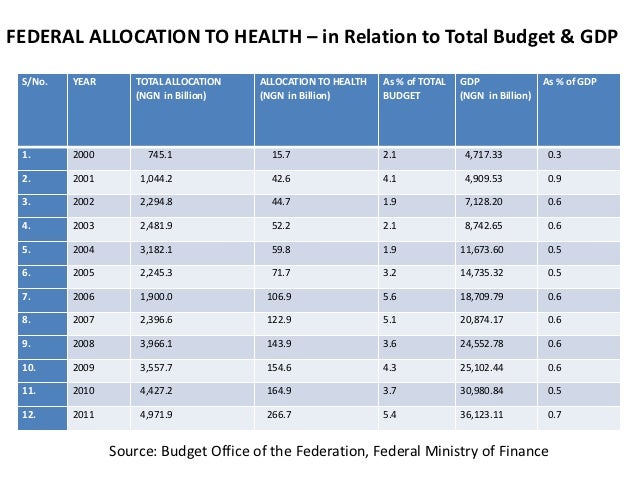
In the case of Nigeria where the current public health budget is shown to be US$25.00 per capita annually, this is the budgetary figure that must be used. Since the maximum allocation for eHealth in any country is about 2.0 % – 3.0 % of the public health budget, this equates to about US$0.50 per capita annually being available for a national PAS/S implementation. When a greater allocation of financial resources is made available to the public health sector, the higher figure will be utilized to determine the extent of additional eHealth services that can be implemented.
The cost of a typical PAS implementation in a Canadian hospital is about US$15.00 per capita annually, and in Jamaica the annual per capita cost of the Heron Technology PAS/S is about US$1.00 annually.
Even in the same country it can be shown clearly that it is the ‘cost’ – not technology – that enables some hospitals to embrace eHealth, yet a large group of other hospitals have no eHealth at all. There are many such examples, however one – namely India – was studied closely by Heron as a result of two trips to India to discuss health sector computerization in both the public and private sectors. The findings showed that all of the 10,000 private hospitals were started into eHealth by the year 2000, yet none of the 14,000 public sector hospitals had even started into computerization, including India’s largest public hospital – a 2,000 bed facility in New Delhi.
# 2 APPLICATION SOFTWARE FUNCTIONALITY
Clearly, the application software implemented must be able to manage properly the application and work flow process that it is designed for – however this is often not the case. Since we are talking about moving the health systems in developing countries from manual paper-based systems that are presently in use, to eHealth, it is critical that the new eHealth systems provide the SAME basic functionality and work flow processes as the manual paper-based systems. If this is not the case then the manual systems must first be replaced, with the functionality of the planned eHealth systems.
Before computerization can start the manual systems and the eHealth systems must be the same, otherwise there would be complete chaos, providing no baseline for the new eHealth systems to be run parallel against, and to provide the same output figures for all computations, etc.
In the case of Commonwealth countries ( Canada, Jamaica and Nigeria) the historical manual paper-based systems have been the same for over one hundred years, thereby ensuring that a PAS/S as offered by Heron Technology does have the required functionality – having been developed in Canada, and subsequently implemented in Jamaica (a developing country) with no software changes being necessary.
It is noted above that when the Philippines tried to implement a USA-developed application software system it failed, for the reasons noted.
# 3 IMPLEMENTATION TIMING/ISSUES
Given the fact that we are herein discussing the implementation of eHealth in the public sector of developing countries, it has been observed that all too often an unrealistic timeline is drawn up to coincide with some political activity. Such a timeline could be positioned to achieve success before a coming election; to complete an implementation prior to the end of the term of office of a government official; or to achieve some other political objective. Such unscientific reasons will decrease the odds of achieving success.
Forty years of experience has shown that the implementation of a national eHealth system must be measured in decades – not years.
About the Author:
Kenneth Nwosu is an eHealth Professional based in Toronto Ontario Canada and can be reached at nwosukc@mcmaster.ca.

















